Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Diagrams / tables | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) images | Peripheral smear description | Peripheral smear images | Positive stains | Histopathologic description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mathison B. Loa loa. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/parasitologyloaloa.html. Accessed December 19th, 2024.
Definition / general
- Loiasis is caused by the filarial nematode, Loa loa (African eye worm)
Essential features
- Loiasis is caused by the filarial nematode, Loa loa, commonly referred to as the African eye worm
- Occurs in west central Africa and is transmitted by flies in the genus Chrysops (deer flies) (Parasit Vectors 2017;10:172)
- Most patients are asymptomatic, however episodic angioedema (Calabar swellings) and ectopic migration of adult worms to the eye can occur
Epidemiology
- Endemic to west central Africa (PLoS Negl Trop Dis 2011;5:e1210)
- Transmission occurs via the bite of deer flies in the genus Chrysops (Parasit Vectors 2017;10:172
- Adult flies use their sharpened mouthparts to lacerate skin and lap up pooling blood
- Infectious filariform (L3, third stage) larvae are deposited on skin and enter the wound made by the feeding flies
- Larvae develop to adults in subcutaneous tissue
- All genders and age groups are at risk
- Patients who live in rain forests and are active outside during the day (when the vectors feed) are at higher risk
Sites
- Adult worms reside between layers of connective tissue under the skin and between fascia that cover muscles
- Ectopic migration of adult worms to the conjunctiva is not uncommon
- Females release microfilariae which migrate to the lymph vessels and eventually the lungs, where they spend most of their time
- Microfilariae migrate to the peripheral blood during midday, when the vectors prefer to feed
Clinical features
- Often asymptomatic
- After several weeks postinfection, angioedema manifesting as localized swellings (Calabar swellings) appear, most commonly in the upper limbs but also the lower limbs and facial area, that are usually red and itchy
- Eosinophilia present
- Migration of wandering adults to the conjunctiva (Pritt: Atlas of Fundamental Infectious Diseases Pathology, 2018)
Diagnosis
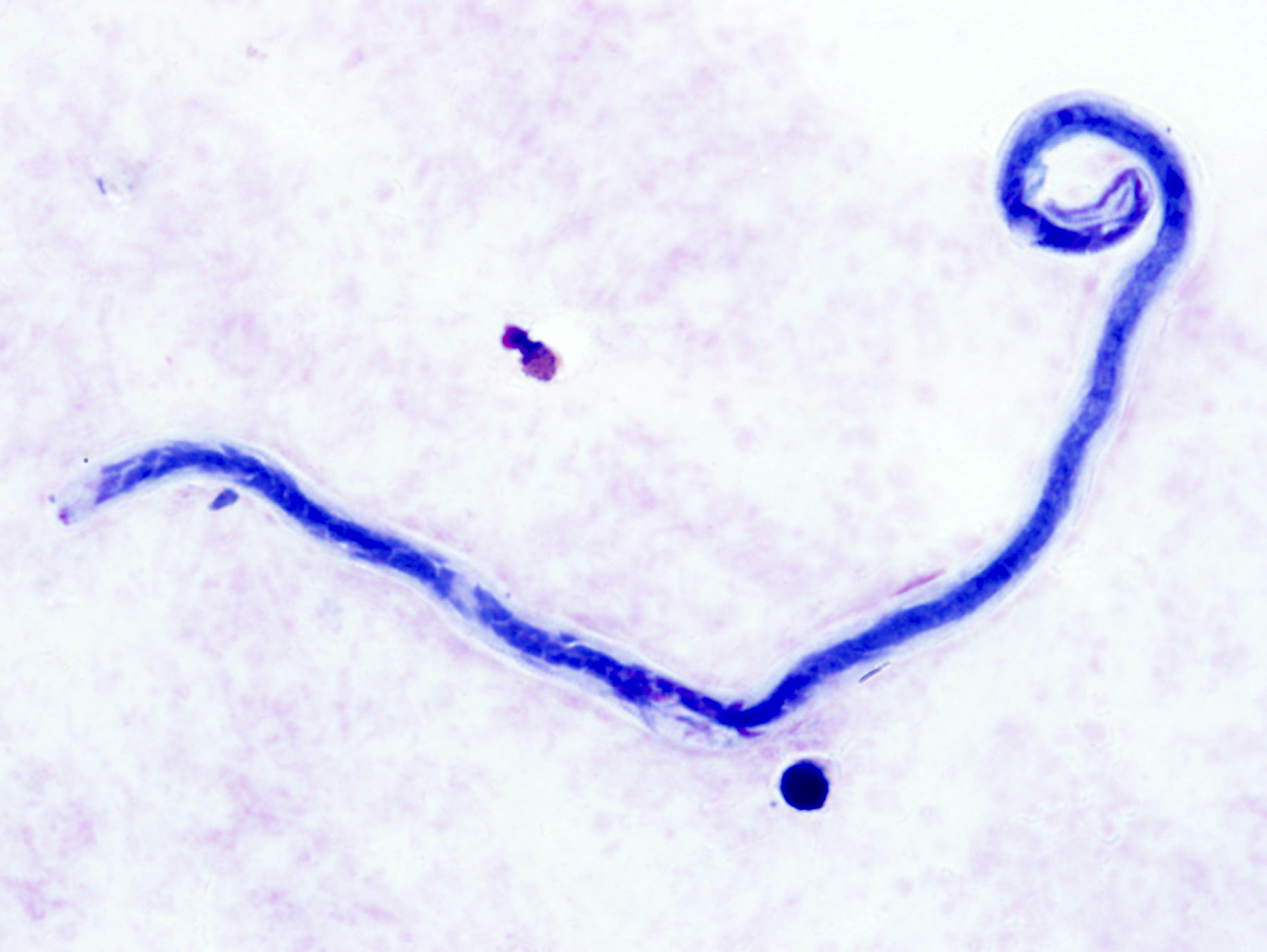
- Diagnosed primarily by the observation of microfilariae on peripheral blood films stained with Giemsa stain, Wright stain or hematoxylin
- Blood should be collected between 10 am and 4 pm, as the microfilariae exhibit diurnal periodicity
- Gross examination of adult worms recovered from the eye (Ash: Atlas of Human Parasitology, 5th Edition, 2007)
- Histopathologic examination of adult worms in subcutaneous biopsy specimens (Pritt: Atlas of Fundamental Infectious Diseases Pathology, 2018)
Case reports
- 25 year old woman returning from Bioko Island, Equatorial Guinea (Emerg Infect Dis 2017;23:160)
- 25 year old woman with gradual loss of vision and a sensation of a moving object in her left eye (PLoS Negl Trop Dis 2016;10:e0004436)
- 27 year old patient with painful red eye (Clin Med Insights Case Rep 2016;9:55)
- 29 year old woman with a reduction of Loa loa microfilaremia, using imatinib (N Engl J Med 2017;377:2095)
- 30 year old African man with a foreign body sensation in his right eye (J Travel Med 2008;15:50)
Treatment
- Drug of choice is diethylcarbamazine (CDC: Parasites - Loiasis [Accessed 12 February 2019])
- For patients with symptomatic loiasis with < 8,000 microfilariae (MF)/mL
- Albendazole may be used for patients with symptomatic loiasis with < 8,000 MF/mL and 2 failed rounds of diethylcarbamazine or symptomatic loiasis with > 8,000 mf/mL to reduce microfilarial burden to < 8,000 mf/mL prior to treatment with diethylcarbamazine
- Alternatively, with microfilarial burden > 8,000 MF/mL, apheresis may be performed prior to diethylcarbamazine treatment
- In the US, diethylcarbamazine can only be obtained through the Centers for Disease Control and Prevention, Atlanta, GA
- Diethylcarbamazine is contraindicated in patients with onchocerciasis due to increased risk of river blindness or exasperated skin disease
Clinical images
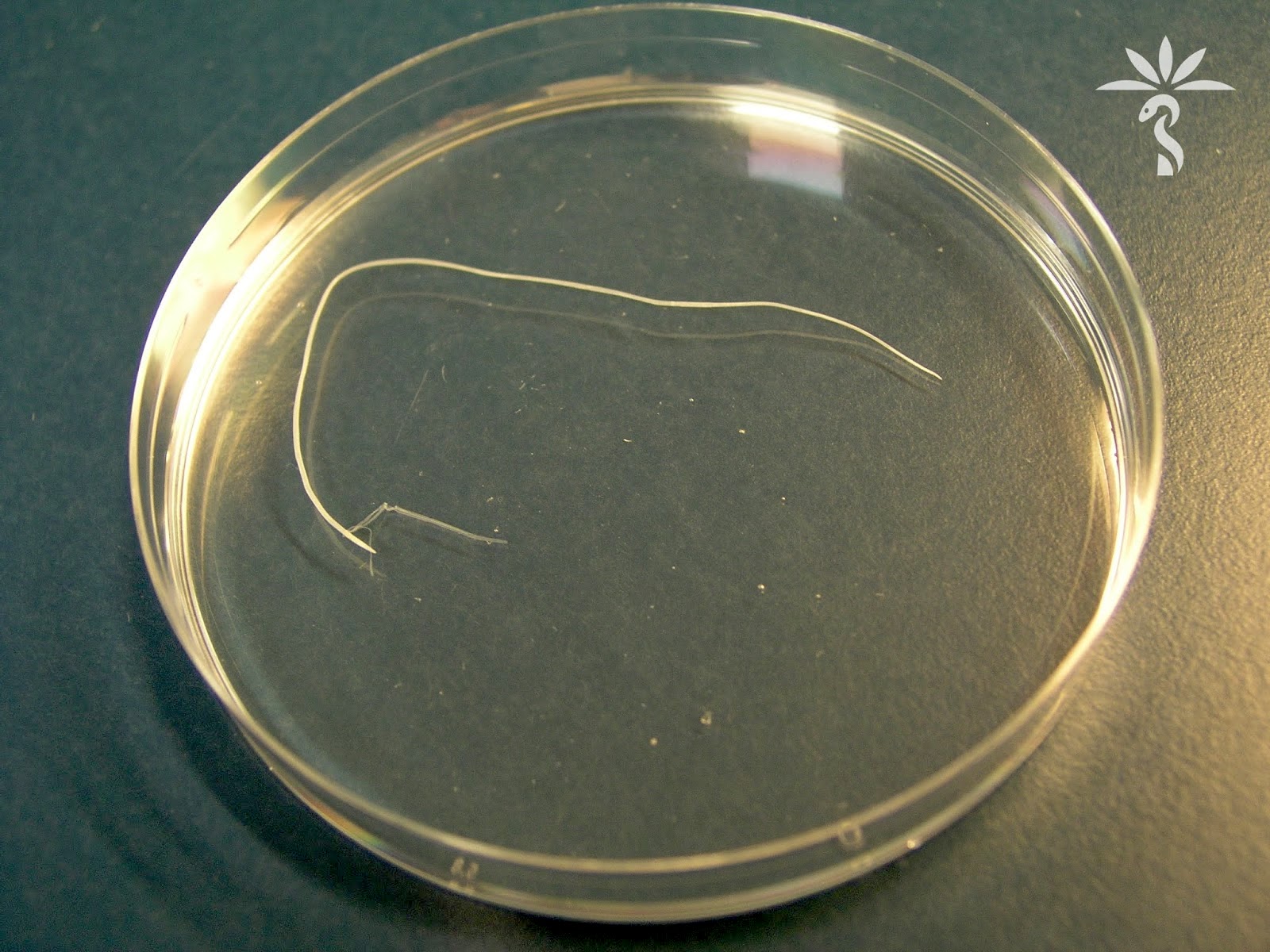
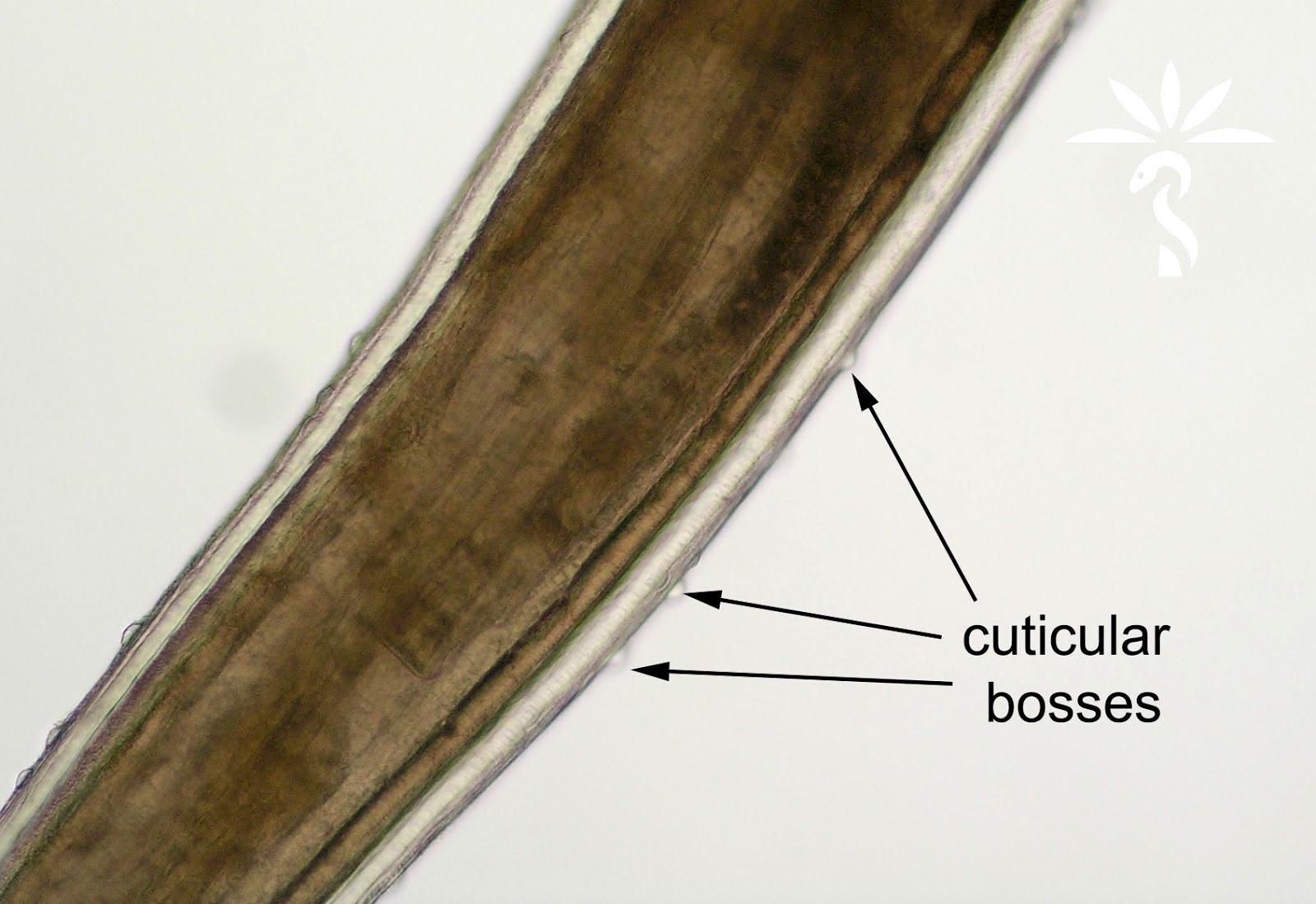
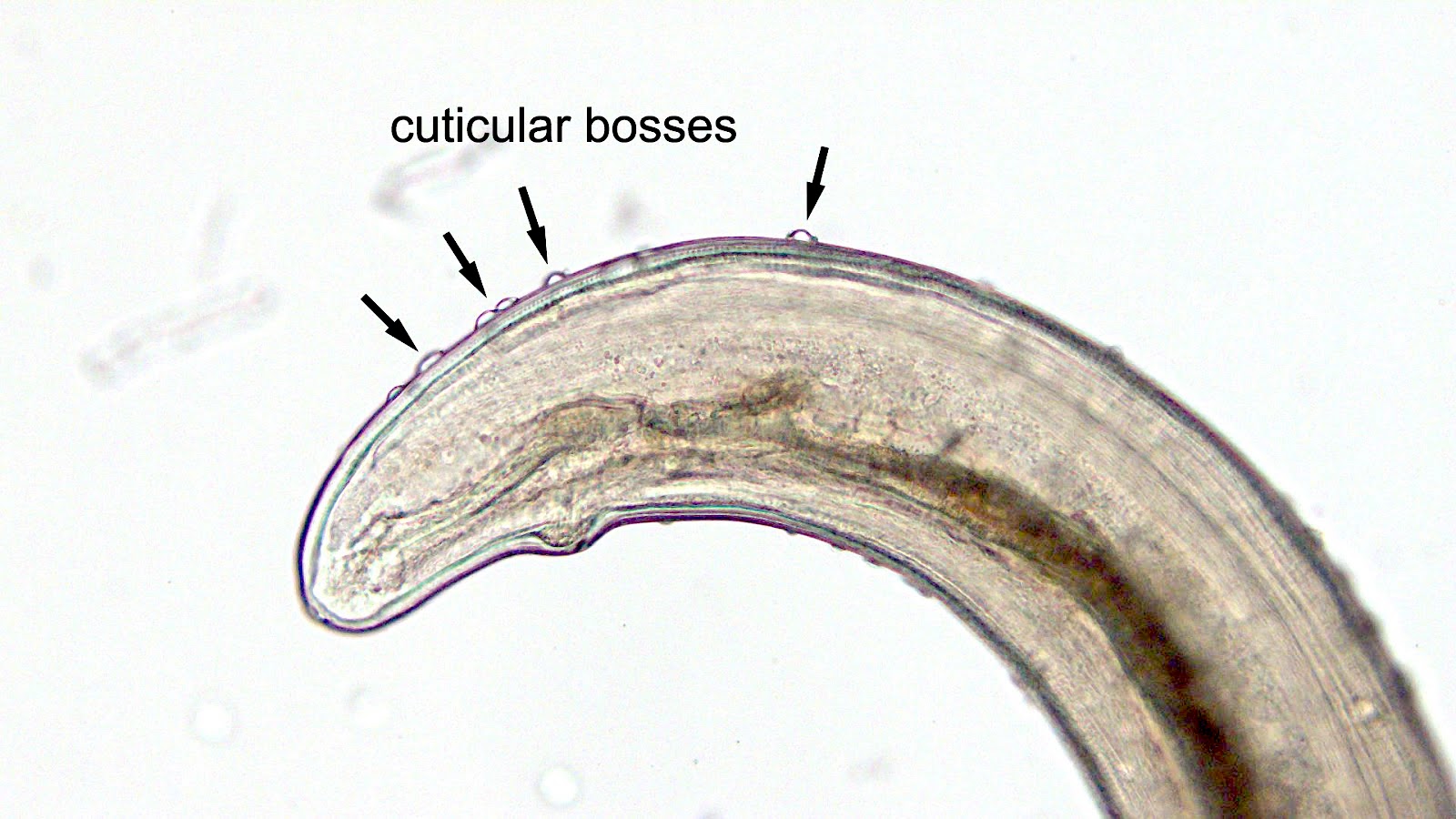
Gross description
- Adult worms recovered from skin or eye specimens are 20 - 24 mm long (males) to 20 - 70 mm long (females) (Ash: Atlas of Human Parasitology, 5th Edition, 2007)
- Cuticle is covered with small, random pimple-like bumps called bosses (Ash: Atlas of Human Parasitology, 5th Edition, 2007)
Microscopic (histologic) images
Peripheral smear description
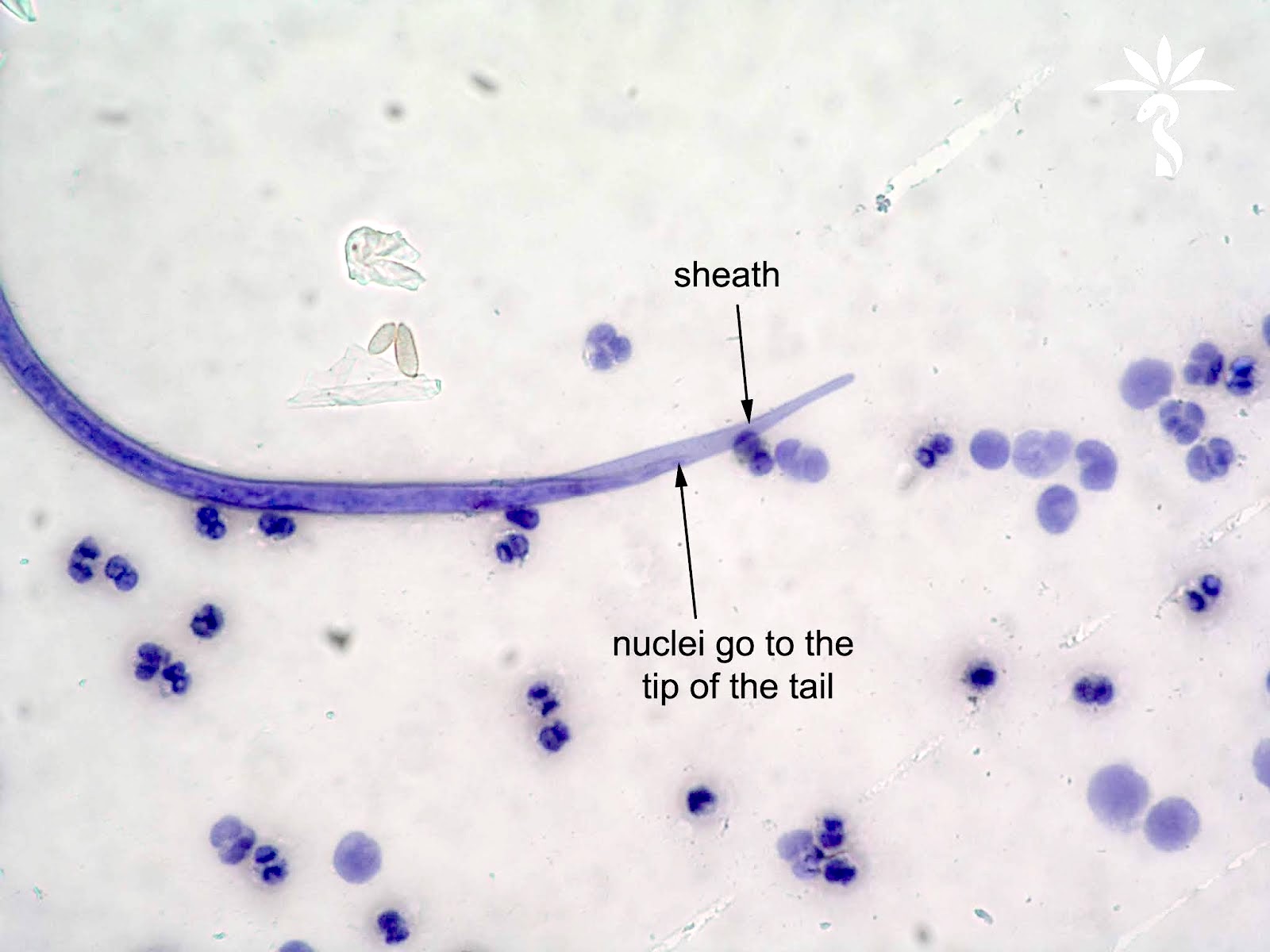
- Microfilariae in stained blood films measure 230 - 250 μm long
- Sheath, when present, is usually unstained with Giemsa at a pH of 7.0 (note: sheaths may be shed during processing and are not always visible on stained blood films)
- Tail is tapered with nuclei irregularly spaced to the tip of the tail
- Compact nuclear column
- Relatively short head space (distance between anterior end of nuclear column and the anterior end of the microfilaria) (Ash: Atlas of Human Parasitology, 5th Edition, 2007)
Peripheral smear images
Positive stains
- Giemsa
- Wright's stain
- Hematoxylin
Histopathologic description
- Thick cuticle lacking longitudinal external ridges and lateral alae (bosses may not show up on sectioned specimens)
- Low, dome shaped lateral chords lacking an internal ridge
- Coelomyarian musculature, with 8 - 12 cells/quadrant
- Developing microfilariae may be observed in utero
- Weak, simple intestine
- Ventral nerve chord not discernible
Differential diagnosis
- Blood from same geographic area:
- Wuchereria bancrofti:
- Larger and may have a sheath
- Tail is anucleate
- Mansonella perstans:
- Smaller (190 - 200 µm in blood films)
- Always lacks a sheath
- Blunt tail with nuclei packed to the end of the tail
- Brugia malayi:
- Endemic to southeastern Asia
- Brugia malayi has a sheath that usually stains pink with Giemsa
- Onchocercerca / Mansonella streptocerca:
- Microfilariae are diagnosed in skin snips and not in peripheral blood
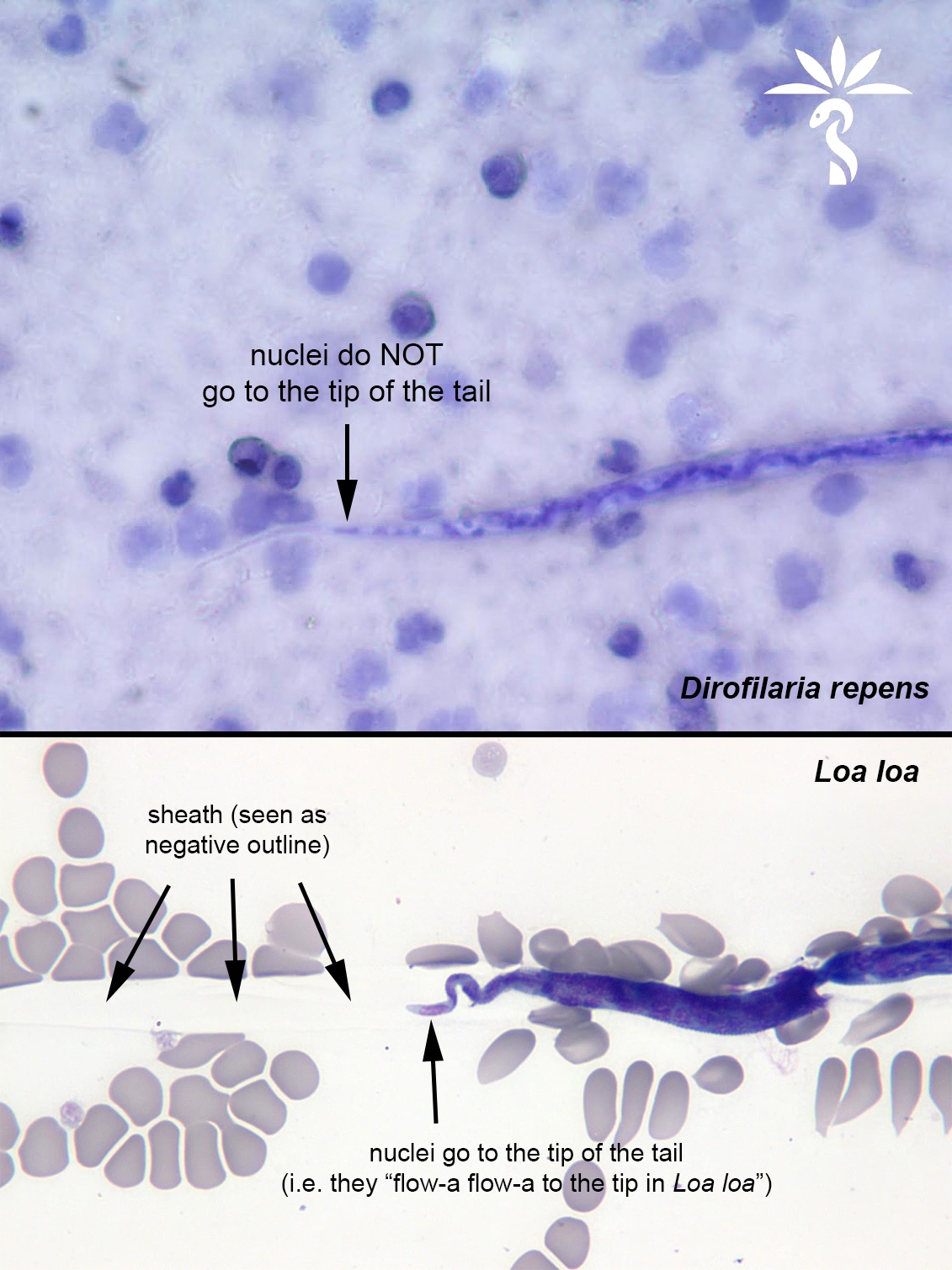
- Dirofilaria:
- Nuclei do not go to the tip of the tail
- Wuchereria bancrofti:
- Skin or eye:
- Dirofilaria:
- Adult recovered from the eye have longitudinal cuticular ridges
- Dirofilaria:
- Biopsy specimens:
- Dirofilaria:
- More numerous and taller muscle cells per quadrant
- Larger more voluminous lateral chords with an internal ridge running along the base of the lateral chords
- External cuticular ridges will appear as short spines around the cuticle in cross section
- Onchocerca volvulus:
- Broad but short lateral chords
- Weak musculature with only 3 - 4 cells per quadrant
- Female usually gravid with characteristic microfilariae in utero
- Gnathostoma:
- Very large, voluminous lateral chords
- Short, boxy muscle cells
- Intestine has large, prominent nucleated cells
- Esophagus is strongly muscled
- Manifest in the human host as larvae only, sexual structures are not advanced
- Dioctophyme renale:
- Prominent ventral nerve chord with U or V shaped arrangement of nuclei
- Lagochilascaris minor:
- Endemic to South America (does not geographically overlap with Loa loa)
- Adults have prominent lateral alae, tall, linear intestinal cells and tall muscle cells, numerous per quadrant
- Dirofilaria:
Additional references
Board review style question #1
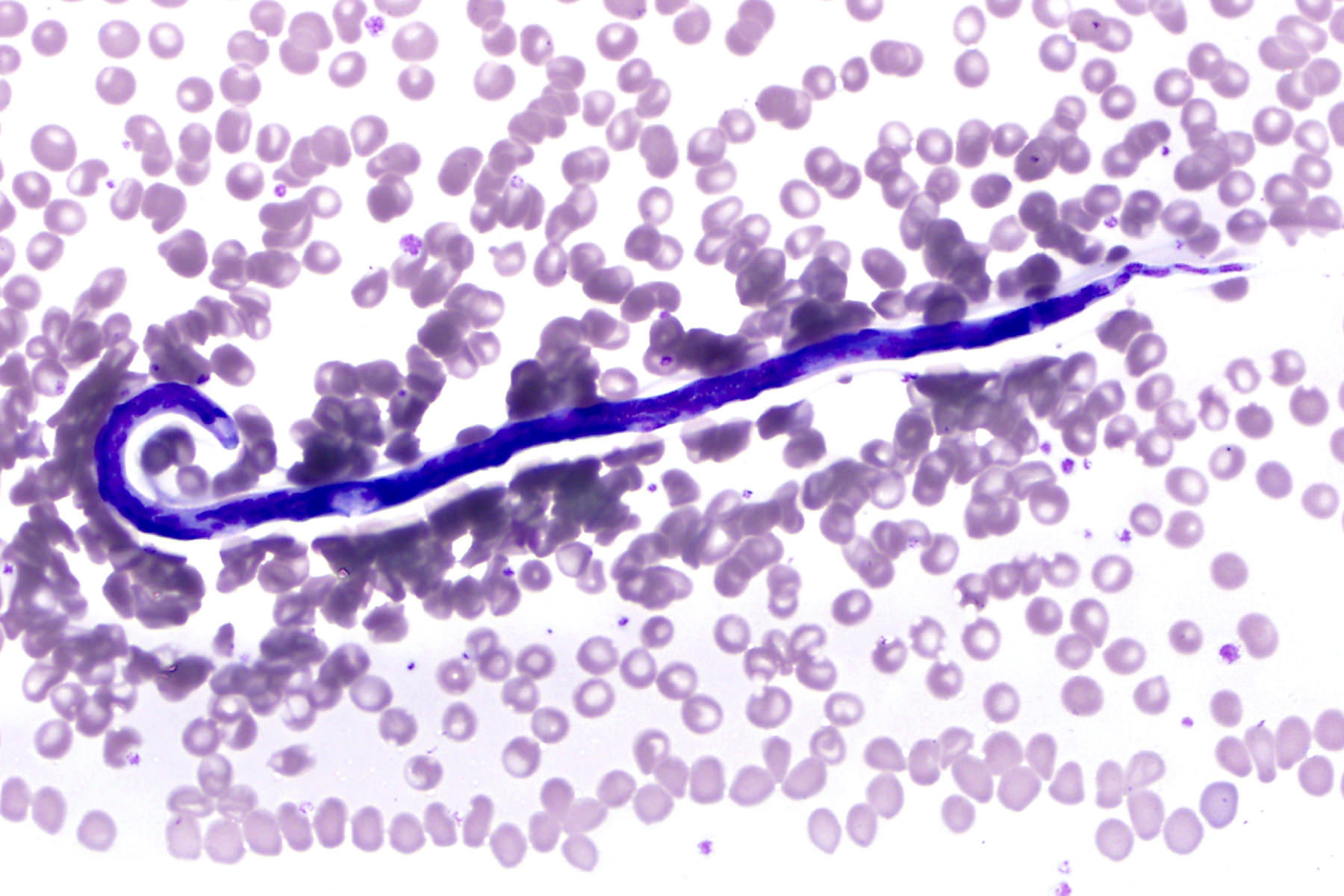
The following object was observed in a thin blood film stained with Giemsa from a traveler returning from Cameroon (Central Africa). What was the source of the infection?
- Bite of a deer fly in the genus Chrysops
- Bite of a mosquito in the genus Anopheles
- Bite of a sand fly in the genus Phlebotomus
- Bite of a tsetse fly in the genus Glossina
Board review style answer #1
A. Loa loa is transmitted by deer flies in the genus Chrysops.
Comment here
Reference: Loa loa (loiasis)
Comment here
Reference: Loa loa (loiasis)
Board review style question #2
While reading a blood film stained with Giemsa (pH 7.0) on a patient with travel to Cameroon (Central Africa), a
microscopist made the following observations: presence of microfilaria measuring 245 micrometers
in length, colorless sheath present and nuclei irregularly spaced to the tip of the tail. What would be
the correct identification for a filarial nematode meeting these criteria?
- Brugia malayi
- Loa loa
- Mansonella perstans
- Wuchereria bancrofti
Board review style answer #2
B. The correct identification would be Loa loa. Diagnostic morphologic features of the microfilariae of
Loa loa include
The epidemiology was also supportive as Loa loa is endemic to west central Africa. Wuchereria bancrofti can be ruled out by the presence of nuclei at the end of the tail. Brugia malayi can be ruled out by the arrangement of tail nuclei, the colorless sheath and geographic location (Brugia species are endemic to southeastern Asia). Mansonella perstans is smaller (190 - 200 micrometers in length) and always lacks a sheath.
Comment here
Reference: Loa loa (loiasis)
- Large size (231 - 250 micrometers in length on stained blood films)
- Presence of a sheath that does not stain with Giemsa (note: sheaths may be shed during processing and are not always visible on stained blood films)
- Compact nuclear column with a short head space (distance between the anterior end of the microfilaria and the start of the nuclear column)
- Tapered tail with nuclei irregularly spaced to the tip of the tail
The epidemiology was also supportive as Loa loa is endemic to west central Africa. Wuchereria bancrofti can be ruled out by the presence of nuclei at the end of the tail. Brugia malayi can be ruled out by the arrangement of tail nuclei, the colorless sheath and geographic location (Brugia species are endemic to southeastern Asia). Mansonella perstans is smaller (190 - 200 micrometers in length) and always lacks a sheath.
Comment here
Reference: Loa loa (loiasis)